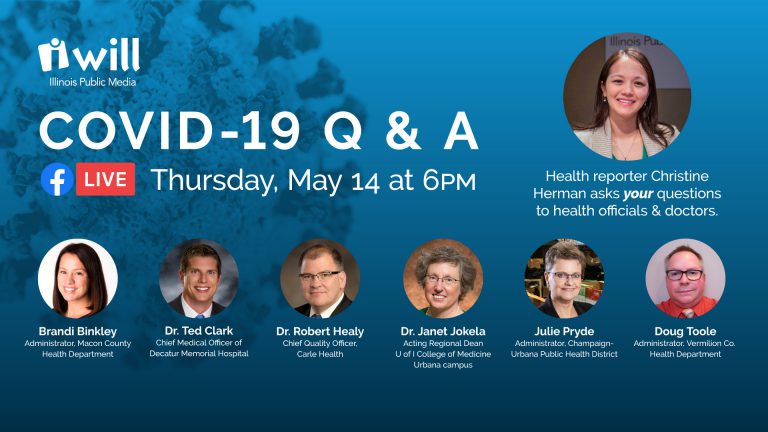
- Status updates from local public health administrators and medical doctors
- COVID-19 immunity, contact tracing, social distancing and face mask guidance
- Antibody testing, advice on reopening the economy, questions about childcare
- Dental care, elective medical procedures, public health services and what’s on the horizon
- Employer responsibilities, where to report issues and final thoughts
COVID-19 immunity
Christine Herman: Let’s dive right into questions. Rosa wants to know: “What information do we have on immunity of COVID-19 once someone has had it?” Dr. Healy, what do we know about immunity against COVID-19 once someone has already contracted the illness?
Dr. Robert Healy: Well, we’re able to do testing now and find out if someone has antibodies, and there’s different types of antibodies but some will show that you have been exposed to COVID in the past. And we’re actually doing that on patients that need that test, which is actually very few.
More importantly, we’re studying or we’re looking at our employees. And we started with the high-risk employees, meaning the people that were at the front lines in the emergency department, and we’re going through to test anyone that wants to be tested eventually for these antibodies.
So that’s the facts, now, what does that mean? Really what it means is if you have a positive antibody (test) it means you’ve been exposed to COVID. That’s all we know right now. We can’t say anything more than that. What we very much hope is that having antibodies will prove to give you some immunity, at least for a number of months, hopefully years, it’d be wonderful if it was lifelong. From things that we know from science for other (coronaviruses), the kind that cause the common cold, that immunity wave wanes off after a few months to a year or two, so that might be what we’re dealing with from COVID. But anything we say about COVID, we have to acknowledge that this is a very unique virus. And we just don’t have the science yet to say what an antibody level will mean to you.
COVID-19 case counts
Christine Herman: The second part of Rosa’s question is: “How accurate are the numbers for current cases?” Julie, we’ve increased the level of testing both locally and across the state over the course of this pandemic, but we still are hearing all the time that there’s not enough testing. Do we know what the reality is in terms of how many people have contracted COVID-19?
Julie Pryde: We believe that there’s at least 10 times as many people that have been infected with this (than reflected in current case counts). You know, it’s all kind of a guessing game at this point, until we get the antibody testing widespread. At the beginning, of course, almost no one could get tested and then as it’s expanded out the testing gets wider, but everybody who had been sick all those months (early on), we just don’t we just don’t know.
Social distancing concerns
Christine Herman: Jessica wants to know: “How can I help my family understand the importance of social distancing and other CDC guidelines? I understand the importance of them for myself, but it is very concerning to see those I love disregarding the guidelines, I am not sure what I can do besides just sharing factual information with them.” Brandi, I wonder if you can chime in with any advice you might have for Jessica?
Brandi Binkley: Yes, definitely. I think this is a struggle for all of us in public health and in the healthcare field right now, especially because we’re really trying so hard every day to get people to take these proactive measures like social distancing, to try to prevent that spread of illness. So I think facts can always be very, very helpful, but if that is not impacting your family the way that you would hope for it to, you know, maybe giving the emotional or personal side of it.
Your family may feel like they are not at risk of having COVID-19, but maybe you are more at risk, or maybe you go and you’re around people at work, or you’re around other people that are in the vulnerable populations, and you don’t want to put them at risk. So, by them not making the choice to social distance or to do things safely with you, as we start moving forward and we’re able to be around more people in a safe way, you know, they have to understand that they’re not just putting themselves at risk, but anybody else that they would come into contact with, and then anyone that you could spread it to.
So, I think that’s something I may be facing with my own extended family, having to explain to them why it’s not just about those of us that might be together in a room, but everyone else with whom we may come into contact. And also it’s really important for us all to lead by example, and I know, you know, everybody tonight is doing that, but it’s important that you know, it’s a culture change, that we’re all doing these things and making it, you know, something that’s normal and comfortable and we’re stressing the importance of this everyone that we love that we work with and that we have contact with.
Enforcement issues
Christine Herman: We got several questions about enforcement issues, mostly about enforcement of the use of masks. Angela wrote in to ask: “Can County Health Department officials enforce the governor’s order? For instance, can they enforce facemasks in retail stores that aren’t enforcing it? Do you have a local lever like a fine or forcing closure, the same way you are able to force compliance with food safety guidelines at restaurants?” Doug, what is the local health department able to do or perhaps not able to do when it comes to enforcement, and what advice would you have for someone who’s concerned about lack of enforcement?
Doug Toole: It’s a really good question. Maybe equating an employee or customer not wearing a mask to some violation of the food code that could make people sick isn’t really a fair way of looking at it. The Illinois food code, and now the FDA food code that we’re using, is written into law. It’s been established for a long time, it’s got the backing of state agencies and a lot of history behind it.
With the executive orders, it’s more of a temporary thing that’s in place right now. So, while we are getting calls from people complaining that I’m going to a retail store or a fast food place, and maybe all the employees aren’t masked. Or is asking like, well, what other steps did they take, is there now a plastic barrier between the employees and the people coming into the store? Are they limiting the number of people coming in the store to make it easier to social distance? You know, what other steps besides masks and gloves maybe are they using to make that happen?
But for customers who are in a place and they’re concerned that the sign may say all customers must wear masks, and they’re seeing people who aren’t, talk to the managers about that? If you’re upset about it, that’s where the change happens. And it’s important for them to know that you may take your business elsewhere if they’re not complying with these things, if they’re not taking this seriously.
Guidance on masks
Christine Herman: David wrote in to ask: “Can people be instructed on how to wear a mask?” Dr. Jokela, can you offer some general guidance on how to properly wear a mask, put it on, take it off? And where would you place people for guidance?
Dr. Janet Jokela: Sure, I’d be happy to. In terms of wearing a mask, there’s a number of different kinds of masks out there and for the general community right now, because of the shortages in the hospital, the cloth face masks would be the ones that we’d be recommending. This helps preserve the surgical masks and N95 masks for use in the hospital where they’re known or suspected COVID patients.

So with the cloth face masks, first of all, there are directions on the CDC’s website for how to make those. With the masks, you want to make sure that they would cover your nose and your mouth, just covering the mouth isn’t enough. And then there would typically be little elastic loops or little ties that you could either slip behind your ears or tie behind your head.
Christine Herman: The CDC website also offers tips there for how to create your own homemade cloth masks from materials you may have at home. So that can be a useful website for people to check out.
Contact tracing
We got a few questions also about contact tracing. Before I get to those, I would like to have one of the public health officials explain what contact tracing is and why it’s important. Julie, can you start us off?
Julie Pryde: Sure. First of all, contact tracing is nothing new. It is, it’s suddenly, you know, the star of the show out there, and everyone’s talking about it. But public health departments all over the world do contact tracing every single day. There are reportable diseases, and when the health department gets a reportable disease, then we basically have different algorithms and different things we do for each type of disease.
So with COVID, when we get a COVID positive, public health is notified by the laboratory or the clinic. And then we call the positive case and we interview them to find out: Where do you work? Who have you been in contact with, and we hope the answer is no one because I’m not supposed to be, but that’s rarely the case. But ideally, you know, other than people at your worksite or people in in your home, we hope that there are no other contacts.
What we do is try to get them to be really honest with us. So we put that person in isolation, and then we contact all of the people that they may have been in contact with. And then we offer them testing and then put them in quarantine either pending test results or until the their incubation period is over. And that’s pretty much what it what it boils down to.
It gets a little trickier when you can’t just do something on the phone, where you have to go out and actually find people and things like that. But I think that, with this, people are understanding that it’s important and that it’s a good thing to tell people who you may have been in contact with to give them a chance to get tested and that helps us shrink it down more and more. And then, during that, if you get a positive test result, then of course you start that process all over and then it just keeps going from there.
Christine Herman: Robin wrote in and she referenced the time that Governor Pritzker earlier this month said that he’d be launching a $40 million contact tracing program. Has that help trickled down to your local departments? Brandi, has that support come available through the state? Or how are you managing otherwise?
Brandi Binkley: We’re still waiting on some more information (about) that entire process, as far as what Governor Pritzker had been discussing and what Dr. Ezike had discussed. As far as this new funding, we do not have that yet. We’re still waiting on additional guidance.
However, as far as for us at the Macon County Health Department, we have people that regularly complete contact tracing activities whenever there is some kind of communicable disease. So we already have that in place. We also had people cross-trained as soon as we started seeing this as an issue that was going to grow much larger more quickly. We did have additional people trained and then we have other divisions within our health department that do have nurses that are ready to be called in for backup.
That being said, to try to kind of advocate for other health departments, not all health departments have, you know, as many nurses as we do, or as many people and if there is a large spike in this, we may not end up having enough people. So we will need additional support, and we may not know exactly what that looks like now, as far as how many people we would need.
And I will tell you, just overall, you know, public health is underfunded, and so when you get to something like this, this stretches you thinner than thin and it’s very difficult to try to staff everything, all of the regular essential life-saving services that public health provides, plus also respond to a pandemic. It’s very difficult, it’s trying,
I think all the health departments that we have been communicating with have done an excellent job of stepping up to the plate and doing everything that they can, but I do think it’s important for people to realize when they take the measures, like social distancing, cloth face coverings, sheltering in place that makes us and the hospitals, etc., be able to manage this in a better way to actually try to prevent more spread of illness and death. Because if we get these huge surges, it’s very difficult for health departments to manage that as well.
Christine Herman: We’ve got one more on contact tracing before we move on to a couple medical questions that have come in. This one’s specifically for Julie: What is Champaign Urbana Public Health District’s opinion on the use of phone apps compared to human contact tracing? So I’m guessing this is talking about using people’s GPS cell phone data to track where they are and if they may have been exposed to someone who has had a confirmed COVID-19 case?
Julie Pryde: Okay, well, first and foremost, I’m a Boomer. So that’s a little above my my skill level how that works. But what we do ask people is to go ahead and look at their own cell phone. And you know, we carry so much data with us right now, and we’ve even done that with foodborne outbreaks, we’ll say, hey, you look back and see where you’ve been where you’ve been spending money. And that helps to jog people’s memory. So we really ask the people to use it themselves to help give us the information.
But there are some really, really neat things coming up, all kinds of apps, all kinds of innovation is coming out of this pandemic, which of course always happens in pandemics. So we are eager to see what some of these are. I can see them being a voluntary thing, like an app that somebody puts on their phone.
The other stuff that we get is more like metadata. So it’s de-identified, we just use it to see (things like): more people are moving out into the parks, less people are in retail, that type of stuff. And so we use it like that. But essentially how we’re using that information right now is just asking people to kind of use their own data to look back and see how things are going and where they’ve been.